ABSTRACT Delve into the nature of pain through the lens of Certified Advanced Rolfer™ and Rolf Movement® Practitioner Alan Richardson. In this article, Richardson distinguishes between acute pain and chronic pain, and highlights how modern understandings of pain have evolved from a purely biomedical model to a biopsychosocial perspective. The role of Rolfing Structural Integration with clients who are experiencing chronic pain include: validation and safety, pain education, body map refinement, graded exposure, and counterirritation. By leveraging the body’s natural capacity for neuroplastic change, Rolfers and structural integration practitioners can enhance recovery from chronic pain.
Prior to the advent of brain, there was no color and no sound in the universe, nor was there any flavor or aroma and probably little sense and no feeling or emotion. Before brains the universe was also free of pain and anxiety.
(Sperry 1981, 2.)
—Roger Wolcott Sperry (1913-1994), American neuropsychologist and neurobiologist, and 1981 Nobel Prize laureate in physiology and medicine.
Many of our Rolfing® Structural Integration clients come to us because of their experience of pain. Often their pain reduces or disappears because of the effectiveness of our specific fascial interventions that help distribute weight and forces more evenly throughout the body. Structural integration reduces stress on specific muscles and joints that may be causing pain. Some clients, however, report persistent pain that does not resolve easily. They may have undergone other treatments, both medical and somatic, and be frustrated because nothing has worked to significantly alleviate their pain. So, what is chronic pain? And how can the Rolfing practitioner help? This article is an attempt to answer these questions.
What is Pain?
The International Association for the Study of Pain (IASP) is a global organization of scientists, clinicians, healthcare providers, and policymakers that has been collaborating since 1974 on bringing relief to those in pain.1 The IASP researchers summarize pain as “an unpleasant sensory and emotional experience associated with or resembling that associated with actual or potential tissue damage” (O’Malley et al. 2024, 1446).
The traditional view of pain is known as the biomedical model, which asserts that pain directly indicates tissue damage or injury (Lugg 2022). This kind of pain is called nociception, meaning that unspecialized free nerve endings are triggered by tissue damage or injury; these nerves initiate the sensation of pain (Purves et al., 2001).
As you can see from the IASP definition, the modern view of pain recognizes pain as a multifaceted experience influenced not only by biological but also psychological and social factors.
Key milestones in this pain research transformation from biomedical to biopsychosocial include:
- Gate control theory (Melzack and Wall 1965) suggested that pain is not just a direct result of sensory input but is modulated by the central nervous system.2
- The biopsychosocial model (Engel 1977) then laid the ground for a more holistic approach to pain management.3
- Advances in neuroscience in the late twentieth to early twenty-first centuries uncovered the complexities of pain processing in the brain and the phenomenon of neuroplasticity, where chronic pain could lead to
lasting changes in the nervous system (Doidge 2007). - The central sensitization concept (Woolf 1983) is where researchers began to understand how the central nervous system becomes hypersensitive to pain signals, leading to persistent pain even in the absence of ongoing tissue damage (Latremoliere and Woolf 2009).
- With the validation of the central sensitization concept, there has been increased recognition and understanding of chronic pain conditions such as fibromyalgia and neuropathic pain, which do not always have clear links to tissue damage (Harte, Harris, and Clauw 2018; Woolf 2011).
Pain is a Complex Phenomenon
Pain can arise without a clear cause, persist after tissue recovery, and occasionally remain absent despite evident injury or pathology. The intensity of pain may not align with the seriousness of the underlying condition, with individuals experiencing similarly severe injuries often reporting differing levels of pain.
The traditional view, that pain is a detector of tissue damage, at first seems reasonable when we consider acute pain. You stub your toe or burn yourself on the stove, feel pain, and there is an obvious response in the tissue, usually reddening and inflammation. It seems as if pain and tissue damage are the same thing, that pain is
tissue damage. If pain were a straightforward detector of tissue damage, however, then shouldn’t the level of pain be proportionate to how dangerous that damage is to
the organism?
Consider the experience Australian neuroscientist G. Lorimer Moseley, PhD, recounted in his widely viewed TEDxAdelaide video on YouTube, Why Things Hurt (2011).
As a boy, Moseley often played outside in tall grass in his Australian landscape and was habituated to the multiple minor scrapes and grazes that came with walking through the territory. Fast forward to his adulthood. While on a hike in tall grass, he feels a painless little nick on his leg, thinks nothing of it, and carries on walking. Soon thereafter, he notices two fang puncture marks on his leg, goes into shock, and has to receive life-saving treatment having been bitten by the deadly Australian Eastern Brown snake.
A few years later, Mosely is hiking again; something scratches the same area of his leg, and he feels an excruciating pain. His pain level and whole-body reaction make him think he was bitten by a snake again. This time, however, the event was a minor scratch from a twig, but the pain level was severe. Context, perception, memory, and pain are inextricably intertwined. How can the pain Moseley felt be so disproportionate to the amount of harm to his organism? The view based on the latest neuroscience is that pain is a protector, not detector, and that pain is not in the tissues but in the central nervous system.
So how is pain produced?
Acute Pain
The pain might have started in the big toe, but the brain is the thing that give you the ouch. Up unti then it is not pain.
(Bryson 2019, 35.)
—Irene Tracey, PhD, head of the Nuffield Department of Clinical Neurosciences at the University of Oxford.
Acute pain normally lasts less than three months, declines with time, analgesics work well, and physical symptoms are normally visible in forms such as redness or swelling (Sizer 2019). With acute pain, the issue is usually in the tissue.
Acute pain is effective as a protective and adaptive mechanism to keep you safe. It prompts an immediate protective reflex response and sympathetic arousal to enhance the body’s ability to defend against potential threats. Acute pain can be caused by inflammation, a tissue response to isolate and repair damaged tissues, recruiting immune cells to the site of injury, and preventing the spread
of infection.
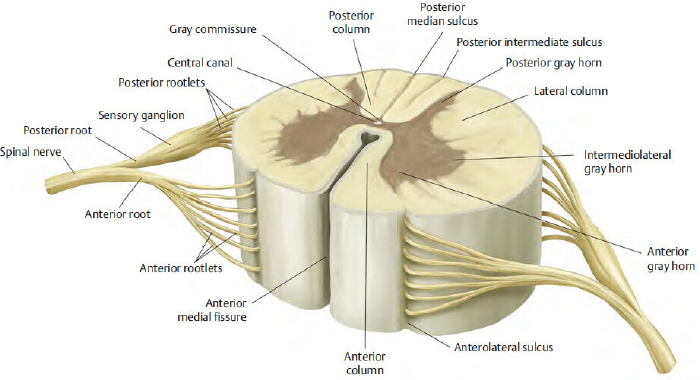
If you stub your toe, your nervous system processes the nociceptive input in the form of neural-electrical information sent from your toe to your central nervous system and then produces pain as an output of the system. As already mentioned, nociceptive input refers to unspecialized free nerve endings called nociceptors, which are sensory receptors, responding to potentially harmful stimuli by sending pain signals to the spinal cord. Nociceptive pain information passes through three neural pathways: from toe to dorsal horn (nociceptive neurons), from the spine to the thalamus (afferent sensory tracts), and from the thalamus to various cortical regions (thalamocortical neurons), where the experience of pain is created.
Pain is a perceptual process and can also be considered an output of the system after the brain has interpreted and integrated not only sensory inputs but emotional and cognitive context as well. Emotional responses to pain include fear, anxiety, and distress, which prompt a motivational drive to escape or alleviate the pain. Cognitive aspects involve the appraisal and interpretation of pain, including the person’s thoughts, beliefs, and attitudes toward the pain, and, as in Moseley’s example in his TEDx talk, can include how past experiences influence the overall meaning assigned to the
pain experience.
Even though acute pain often reflects tissue damage, the intensity of pain an individual feels is sometimes disproportionate to the amount of actual damage. In cases of hypersensitivity to pain, sensory input is modified by context. Nociception may be present, but it is not necessary nor sufficient for pain to exist. As an example of nociception without pain, most people have had the experience of noticing a cut or a bruise after the event, having felt no pain at all.4 There are extreme examples of stress-induced analgesia, where no pain is experienced in spite of extensive tissue damage, such as soldiers with horrific wounds who feel no pain in the heat of battle. It can go the other way, too, where there is pain without nociception. As in the case of a British builder who was in excruciating agony when a nail pierced all the way through his boot. He was convinced that the nail had skewered his foot, only for the doctors to peel off the boot to reveal that the nail had passed between his toes without so much as a scratch to his foot.
These mismatches between pain and tissue damage occur because the purpose of pain is to protect the organism, not to detect tissue damage. The brain makes its best guess based on various inputs and creates an experience of pain that is proportionate to the level of perceived threat. In the example of the wounded soldiers, the brain decides not to create the experience of pain because being immobilized by pain in the heat of battle would be more threatening than keeping moving to escape or defend oneself. The brain chooses the response most likely to ensure survival. Conversely, in the case of the builder, the strong visual information of a nail through the boot causes the brain to create the perception of pain to motivate the appropriate response for the severe injury it believes has occurred.
In the words of Giandomenico (GD) Iannetti, PhD, a sensory neuroscientist at University College London, with acute pain, “generally, you feel what is useful to feel” (Young 2021, 249). Pain is not an objective thing that can be identified in the body. It is an experience produced by the brain, more like an action signal than a detector of tissue damage. This distinction is crucial when it comes to treating people with chronic pain.
Chronic Pain
It’s clear that believing that the pain equals damage actually worsens the pain, whereas treatments that provide knowledge, confidence [sic] and hope really can cure.
(Lyman 2021, 162.)
Our body is like a beautiful, intricate garden. Persistent pain is like a thorny weed. It feeds on soil – unchangeable factors such as past tissue damage, past trauma, upbringing [sic] and genetics. But to grow it also needs to be watered – with stress and inflammation: psychological stress, smoking, a poor diet, insomnia, a lack of exercise, anxiety and social isolation, to name a few.”
(Lyman 2021, 179.)
—Monty Lyman, MD, is an author and research fellow at the University of Oxford.
Chronic pain is synonymous with persistent pain. Chronic pain normally lasts more than three months, the pain level goes up and down, analgesics are less effective, and it is often invisible. The issue is in the nervous system rather than the tissues. (Sizer 2019, 35.)
Unlike acute pain, chronic pain often exists without any detectable tissue damage, in which case it can be classified as nociplastic
pain, where the central nervous system produces the experience of pain without clear tissue damage. This is the central sensitization process mentioned earlier, where the pain circuitry in the central nervous system is amplified, and the pain experienced is independent of peripheral injury or inflammation (Harte, Harris, and Clauw 2018). If the pain pathway is hyperactivated centrally over time, then a low threshold of sensation peripherally could trigger the experience of extreme pain. While central sensitization is considered real pain by the medical community now, there was a time when physicians believed “that pain in the absence of pathology was simply due to individuals seeking work or insurance-related compensation, opioid drug seekers, and patients with psychiatric disturbances; i.e. malingerers, liars [sic] and hysterics” (Woolf 2011, 54).
Chronic pain is a learned response by the neuroplastic brain and central nervous system causing the experience of pain to persist long after the injury has healed. Because of central sensitization, also called pain wind-up, the pain threshold is lowered and the person’s nervous system is more responsive to experience any sensory input as pain. Pain is a product or output of the predictive brain.5 In chronic pain, the pain has stopped being the symptom and has become the disease.
An extreme example of nociplastic pain is phantom limb pain, where the sufferer feels the sensation of pain as if the amputated limb were still attached to their body. Indian-American neuroscientist Vilayanur S. Ramachandran, MD, PhD, has published innovative research on neuroplasticity and phantom limb pain, documented in his 1998 book Phantoms in the Brain, co-authored with Sandra Blakeslee. Ramachandran worked with mirrors, placing them so the participants suffering from phantom limb pain would see the reflection of their intact limb in place of their missing limb. The brain would think the missing limb had returned. When the brain could perceive the mirror image, it was given the illusion of no tissue damage, the pain signal in the missing limb would subside, and many amputees report no pain after several treatments with the mirrors.
The whole body is a phantom, one that your brain has constructed purely for convenience.
(Lyman 2021, 193.)
Most musculoskeletal injuries heal within three months of the onset of pain, yet I have seen clients in my practice whose pain started with an injury and persisted for much longer. How is it possible for an injury to cause pain so long after the initial event? It is because pain protects against a perceived
threat, not an actual threat, and the brain’s perception of reality in this regard can simply be incorrect. In the words of Andy Clark, PhD, professor of Cognitive Philosophy at the University of Sussex, our “predictive brains are guessing machines, proactively anticipating signals from the body and the surrounding world. That guessing is only as good as the assumptions it makes, and even a well-informed best guess will frequently miss the mark” (Clark 2023, xiii). Many factors other than tissue damage influence the brain’s decision whether or not to create pain, such as stress, anxiety, fear, memory, social exclusion, and feelings of helplessness.
If you feel a muscle twinge in your lower back, it is easy to believe that your spine is damaged, especially when you have been exposed to ominous-sounding jargon such as ‘slipped disc’, ‘bulging disc’, and ‘bone on bone’. Your brain assumes something serious has occurred, so you become fearful and avoid movements that demand even minor effort from your back. You may start to brace yourself in order to protect the ‘injury’ and unwittingly create a constellation of tension around the painful area that only serves to perpetuate the discomfort. Before long, your avoidant behavior occurs in anticipation of pain and not in response to it. You become anxious and irritable, which only seems to further worsen the pain. Your expectation of pain perpetuates a vicious cycle.
There is a poor correlation between pain and structural anomalies in the back. In a 2015 study published in the American Journal of Neuroradiology, 37% of pain-free twenty-year-olds and 96% of pain-free eighty-year-olds had signs of ‘disc degeneration’ on scans (Brinjikji et al. 2015). The problem is that correlation can be mistaken for causation. People with back pain may receive surgery with mixed results when the original motivation for the surgery was the finding of a degenerated or bulging disc on an MRI scan. Often, people seek surgery before exploring other methods of help.
The good news is that the neuroplastic brain changes according to input. Just as the brain can rewire itself in a learned response to create chronic pain, it can also rewire itself in order to recover from chronic pain.
How the Rolfing Practitioner can help with Chronic Pain
What helps with chronic pain is adopting a wide perspective. This means looking at the whole of life, not just the medical aspects. When you do this, you may see something important that has been missed. You may find a solution to one bit of the puzzle and therefore improve the whole.
(Sizer 2019, 23.)
Pain causes us to withdraw from danger, but persistent pain causes us to withdraw from life.
(Lyman 2021, 184.)
Chronic pain affects many aspects of a person’s life such as sleep, mood, confidence, fitness, relationships, finance, and work. People feel frustrated and fearful that their pain is not getting better or is even getting worse. They can feel helpless and guilty that they cannot do things they feel they should be able to do. Perhaps the most frequent emotion attached to chronic pain is fear: fear of the pain, fear of damage, fear that this situation is going to last for ever, or fear related to any one of the other areas of life affected by the pain. This accumulation of factors creates stress, which in turn exacerbates the pain.
As Rolfers and structural integration practitioners, we are in a good position to help our clients with chronic pain in a variety of ways: 1. Validation and safety within the therapeutic relationship, 2. Pain education, 3. Refinement of body maps, 4. Graded exposure, and 5. Counterirritation.
1. Validation and Safety within the Therapeutic Relationship
As Lorimer Moseley affirmed on The Thinking Practitioner Podcast (Luchau and Lowe 2022), “Our advantage is in the relationship.” As we take the client through the ten-session series of the Rolfing® Structural Integration paradigm, we have time to get to know them and create a therapeutic environment that supports their holistic healing process (Richardson 2024).
Many people who suffer from chronic pain have run the gamut of medical tests and are told that there is no reason for their pain, that their pain is somehow not real, and that they should just ignore it. Labelling pain as not real because no tissue damage can be found on a test can be extremely unhelpful for the pain sufferer who feels that no one believes them and they may also become even more fearful that there is some mysterious physical damage in their body that even modern medical tests are unable to find.
Chronic pain is most definitely real. If no tissue damage has been discovered by a test, this does not mean that the pain “is all in your head” (a phrase that seems to imply unnecessary complaining or even feigning), nor is it something that can be made to disappear merely by thinking it away. We can start to help a client who arrives at our practice suffering from chronic pain by listening to their story, empathizing, and validating the reality of their pain.
We should resist jumping to conclusions or claiming we have the solution to their pain. They have probably heard all this before: “It’s probably a muscle knot, or a rotated vertebra, or a muscle imbalance,” yet they are still in pain. We may have ideas about how we can help them that we can share with them, but initially we must simply validate their experience. Possibly the most important thing we can say in the initial interview, while developing the foundations for
a safe therapeutic relationship, is “That must be really difficult for you. I am so sorry you have had to go through that.”
Here is Dr. Rangan Chatterjee, reporting the words of his colleague, a respected spinal surgeon in the United Kingdom, on his Feel Better, Live More Podcast (2022, 1:27:42):
“The most important thing that I do for my patients when they come to see me is I listen to them . . . surgery’s great for acute cases where we can see something’s going on, but for a lot of the time we just don’t need to do it. For these people with pain, what they need is to feel heard and validated.”
The safety of the therapeutic container is paramount with all clients, but especially in cases of chronic pain. The pain is a
result of the brain’s response to a perceived threat. Part of the healing journey is to retrain the autonomic nervous system to come out of the sympathetic fight, flight, or freeze state and to relax. It is good practice to clearly express to the client that it is important that they feel safe and comfortable communicating how they are feeling. Threat increases pain, safety decreases it.
As Ida Rolf, PhD (1896-1979) wrote
(1989, 202):
So many therapists are striking at the pattern of disease, instead of supporting the pattern of health. One of the things that you as Rolfers must always emphasize is that you are not practitioners curing disease; you are practitioners invoking health.
The vital question we and our client can ask together is, “How can we promote health?”
2. Pain Education
If people living with persistent pain are given a sense of controlled empowerment, the intensity and unpleasantness of the pain should diminish. Clearly, the best way of doing this is by explaining what pain is and what it isn’t.
(Lyman 2021, 93.)
Educating clients about chronic pain can help their recovery, and Rolfers and structural integration practitioners are well-placed to do this. Education modifies the output of pain by changing the cognitive and emotional inputs, such as the sense of threat and anxiety about the pain, and unnecessary fear of healthy movement. Many people who suffer from chronic pain have unsupported ideas about pain, such as the pain in their knee is “bone on bone,” they “have the neck of an old person,” or they are powerless to change their pain. Education about pain can help to dispel these myths and reassure pain sufferers that their body is not broken.
Professor Lorimer Moseley with the University of South Australia, whose TEDx talk I mentioned earlier, is also coauthor of Explain
Pain (Butler and Moseley 2013), a valuable resource for all manual therapists, and has made excellent online resources available to the public to learn about pain science, which he presents as a website: The Pain Revolution. [See www.painrevolution.org.] Moseley is committed to sharing pain science discoveries with the public with free resources (see www.painrevolution.org/newresources).
The Pain Revolution website is in a neat format, which makes it easy for Rolfers and structural integration practitioners to share clear and accurate information about pain with clients over the course of the Ten Series. The following four pain facts come from an eleven-year study that investigated what were the most important facts people suffering from chronic pain valued learning during their recovery. I share these four essential pain facts as examples that could be a part of the education we can offer our clients (see www.painrevolution.org/painfacts):
The Four Essential Pain Facts:
i. Pain protects us and promotes healing,
ii. Persistent pain overprotects us and prevents recovery,
iii. Many factors influence pain,
iv. There are many ways to reduce pain and promote recovery.
i. Pain Protects Us and Promotes Healing
We can imagine pain being like a cliff, where the body knows falling off a cliff brings harm to the tissues. Pain arises when we have fallen over the cliff and injured ourselves, but pain also arises when we are near the edge of the cliff, when there is a high risk of injury. In this way, pain protects us, like a barrier that prevents us from getting too close to the edge of the cliff. When we get injured, it’s usually because we quickly bypassed or gradually slipped past the pain-barrier information at the edge of the cliff.
Injury causes pain because damaged cells and inflamed tissues are more sensitive than normal. In the cliff analogy, this heightened sensitivity of being injured moves the barrier further away from the cliff’s edge, so the pain will likely prevent you from even approaching the point where you might cause further damage. Pain keeps you safe from more serious harm. Normally, the inflammation resolves, sensitivity reduces, and the protective barrier returns to its normal place closer to the cliff’s edge, where you can once again enjoy the view (McKechnie 2022).
ii. Persistent Pain Overprotects Us and Prevents Recovery
Clients often think their chronic pain means that they have unresolved damage in their bodies. If a careful medical evaluation shows no injury or clear pathology, we can point out that chronic pain often occurs because of hypersensitivity caused by their nervous system being too enthusiastic in doing its job of protecting them.
The encouraging news is that because of neuroplasticity, just as the pain system can learn to be overprotective, it can also learn to return to a more reasonable level of protection. The phrase neurons that fire together, wire together [Hebb’s law] encapsulates this capacity of the brain and nervous system to learn from, and adapt to, changes in sensory information, thoughts, or actions (Hebb 1949).
iii. Many Factors Influence Pain
. . . we have the ability to regulate our own physiology, including some of the so-called involuntary functions of the body and brain, through such basic activities as breathing, moving, and touching.
(van der Kolk 2014, 38.)
Clients may think that their tissues cause their chronic pain. While it is true that tissue irritation, excessive loads, and inflammation can be a cause of pain, we also know that other factors such as memory, fatigue, negative predictions, poor nutrition, past traumas, and especially stress can contribute to chronic pain. It is useful to talk to clients about such lifestyle factors that may be relevant to their condition and we can share some of the many scientific studies showing how pain can be modified by emotional and cognitive factors.
Here are some examples:
A 2018 study led by Tor D. Wager, PhD with the Department of Psychology and Neuroscience at the University of Colorado, Boulder, placed participants in an fMRI and showed them visual cues of either the word ‘high’ or ‘low’ while they were subjected to blasts of high or low heat (Kragel et al. 2018). Although there was actually no correlation between the verbal cue and the heat intensity, participants felt more pain when they saw the word ‘high’ regardless of how hot the stimulus was. The experiment shows how expectation affects
pain perception.
In a study described in the book Unlearn Your Pain (Schubiner and Betzold 2019), volunteers wore a bracelet that gave electric shocks. Before receiving the electric shocks, all participants were given a pill that they were told was a new painkilling medication, similar to codeine but faster acting. Half of the people were told that the pill cost $2.50 per pill, and the other half were told that each pill cost ten cents. All the pills were, in fact, placebos. The people who received the supposedly expensive pill reported feeling significantly less pain than the other participants, which again shows the power of expectation to modify the pain experience.
In another study described in Unlearn Your Pain (Schubiner and Betzold 2019), people with chronic hand pain due to complex regional pain syndrome were shown pictures of hands in various positions. When they were asked to imagine moving their own hand into the same positions as seen in the pictures, results showed increased pain, and swelling in their hands. This shows how imaginative input can have a significant effect on how we feel pain.
iv. There are Many Ways to Reduce Pain and Promote Recovery
The process of undergoing the Rolfing Ten Series™ can significantly help clients to retrain their pain system towards normal because of refinement of body maps, graded exposure, and counterirritation (explained below). In addition to this, it can be useful to hold the space for an open dialogue with the client during their Rolfing session about how lifestyle can influence their experience of pain. The most common relevant talking points are stress, exercise, sleep, and diet.
Clients usually appreciate when we show genuine interest in their well-being and also when we are willing to collaborate by recommending specialists beyond our scope of expertise, such as yoga and Pilates teachers, nutritionists, somatic experiencing® practitioners, craniosacral therapists, and/or acupuncturists. (Of course, some Rolfers and structural integration practitioners are also trained in these modalities.) It can be appropriate to sometimes share information based on personal experience, such as, in my case, how meditation, mindfulness, and exercise help to reduce my stress levels.
Also, having a handy digital resources catalog to text or email to clients with relevant TED talks and websites to share with clients is recommended. An example of this appears at the end of this article.
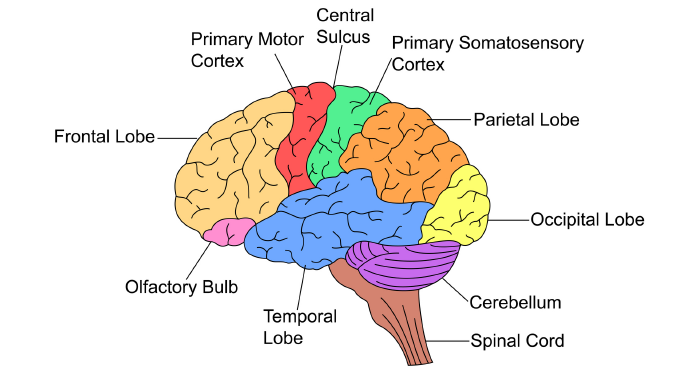
Photo credit: mrhighsky with istockphoto.com.
3. Refinement of Body Maps
The brain’s representation of the body in the sensorimotor cortex is often referred to as a body map, or sensorimotor map. Chronic pain conditions can lead to persistent neuroplastic alterations in the way the brain represents and processes sensory input, potentially leading to distorted body maps, sometimes referred to as “smudging” of body maps.6
In the words of author, blogger, manual and movement therapist Todd Hargrove (2019, 107):
Imprecision is one reason why chronic pain can spread beyond the area of actual tissue damage, move from one area to another, or become more difficult to locate in a specific area.
Hargrove (2019) points out that chronic pain sufferers have been shown to have difficulty in tasks that require accurate perception of body location and motor control. However, studies have shown that sensory discrimination training helps patients reinstate brain precision. The goal of such training is to enhance the brain’s ability to distinguish between different sensory inputs, which can help reduce pain perception. Techniques used include two-point discrimination, where patients practice distinguishing between two points of touch on the patient’s skin that are progressively moved closer together, and graphesthesia where patients recognize letters or numbers traced on their skin with a finger or blunt object.
Another example of sensory discrimination training being used to help reduce chronic pain is the thermal grill illusion; the index finger and ring finger are placed in warm water, and the middle finger in cold water. The unusual sensory input causes people to feel that their middle finger is in painfully hot water. However, pain levels were cut by 64% when subjects were able to press their fingers together; this is because the brain received sensory information to correct the sensorimotor mismatch (Hargrove 2019).
Receiving skilled touch over many areas of the body throughout the Rolfing Ten Series is an excellent way to provide rich sensory somatic information to the brain and nervous system in order to refine the body maps. Clients frequently report an increased awareness of a body part and make comments such as, “Wow, I didn’t even realize that I had a muscle there!” Indeed, a general increase in body awareness and feeling of being more identified with their body is extremely common for Rolfing clients. Incidentally, this strengthening of body awareness sometimes brings an increased awareness of one’s personal boundaries and can possibly explain why some clients report improvements in confidence and self-esteem.
If inaccurate body maps contribute to chronic pain, as the evidence suggests, then it follows that the rich sensory information provided by Rolfing Structural Integration can help refine these maps and contribute to chronic pain recovery. We can talk to clients as they go through the Ten Series to help them understand the role of touch as reorganizational information for the central nervous system in relation to their chronic pain recovery. Inviting the body’s nature of neuroplasticity to lead toward lessening the experience of pain. There are also many somatic explorations within the Rolf Movement® training that are very effective at refining perception and
body maps.
4. Graded Exposure
Graded exposure is “the progressive introduction of threatening movements or other stimuli . . . in a way that causes the nervous system to become less threatened [by the stimuli]” (Hargrove 2019, 114). Again, as Rolfers and structural integration practitioners, we are in a good position to help clients with chronic pain by using graded exposure through touch and movement. The application of careful, focused touch on specific hypersensitive areas of the body with the intention of dialing down the hypersensitivity is part of the overall project within the Rolfing Ten Series. In our work, we are bringing all parts of the body into congruence with each other and with the body as a whole.
So, how can we reduce hypersensitivity? Once a hypersensitive area of the body is identified, we have an opportunity to frame the discomfort in terms that invite the client’s curiosity and participation. We could say, “It is clear that your nervous system is protecting you in this area. Let’s see if we can help it feel safer.” We can cooperate with our client to contact the area carefully and precisely, with the appropriate dosage of pressure and timing, in order to reduce perceived threat. The client can be invited to direct their breath into the area as a way to meet the touch, which will reduce the sense of threat.
It is valuable to encourage clients to give ongoing feedback and guide the practitioner’s touch to where they feel it is most needed. They can help identify what is a tolerable level of pressure and what is not; this serves to strengthen the client’s sense of agency and control. (Remember: helplessness and lack of control can be contributory factors in chronic pain.) A number scale between one and ten, where ten is the highest pain level and one is the lowest, can be useful to compare the level of pain experienced before and after the intervention. As the client is able to relax and the level of perceived threat is dialed down, they will often report a lower level of discomfort even though the same pressure of touch is being applied. Using a graded exposure approach when touching sensitive areas is an effective way to give the client’s brain good news about the health and capacity of their body.
5. Counterirritation
Rolfing sessions can also reduce pain perception by counterirritation, which is where tactile stimuli in the body’s connective tissue induce descending inhibition, a mechanism by which the brain suppresses the transmission of pain signals in the spinal cord.4 The descending inhibitory pathways release neurotransmitters that act on receptors in the spinal cord to inhibit the activity of pain-transmitting neurons, down regulating nociception.
Descending inhibition occurs in the context of ‘good pain’, or hedonic pain, where the nociceptive stimulus is caused by something that the brain considers to be healthy to the organism, or, in the words of Todd Hargrove (2019, 105), “ ... the brain’s opinions about the particular stimulus help determine how it gets processed even at the level of the spinal cord.” So when the client feels safe, trusts the practitioner, and believes the Rolfing intervention to be beneficial, descending inhibition enables them to perceive the deep tactile pressure as a good feeling, albeit a little uncomfortable, because an important area of tension in the body is being addressed. In other words, the expectation that the stimulus will reduce pain increases the effectiveness of descending inhibition to reduce pain
and hypersensitivity.
Conclusion
Between the stimulus and response there is a space. In that space is our power to choose our response. In our response lies our growth and freedom.
(Frankl 1959, unknown page number).
—Viktor Frankl, MD, PhD, neurologist, psychiatrist, philosopher, and author.
In The Thinking Practitioner Podcast, episode 111, which was the inspiration for this article, Lorimer Moseley makes a bold challenge to somatic practitioners. He says: “You are in this job. You have a responsibility to people to be good at it” (Luchau and Loewe 2022, 44:07) That includes educating ourselves about pain so that we can be part of a transformational process for our clients’ chronic pain.
Within the context of the Rolfing Ten Series, with its comprehensive layered treatment of the whole body, we are able to use our skilled touch to provide a rich source of sensorial information capable of tuning down the nervous system of our clients from a state of red alert to one of rest and repair. Chronic pain is a learned response of the nervous system that can be unlearned, and an essential part of our role as somatic practitioners is to help our clients do this.
Resources Catalogue
TED Talks and TEDx about Pain
Lorimer Moseley – TEDxAdelaide (November 22, 2011) – Why Things Hurt (15 mins)
https://www.youtube.com/watch?v=gwd-wLdIHjs
Elliot Krane – TED Talks (May 19, 2011) – The Mystery of Chronic Pain (8 mins)
https://www.youtube.com/watch?v=J6--CMhcCfQ
Lauren Cannell – TEDxHobart (June 12, 2023) – A New Way to Think about Pain (16 mins)
https://www.youtube.com/watch?v=ruKVTOK8gTg
Julia Gover – TEDxNorthwich (August 21, 2019) – Pain an the Brain (11 mins)
https://www.youtube.com/watch?v=zR-1M95Kthw
Sid Anandkumar – TEDxChilliwack – Low Back Pain: Myths vs Facts (14 mins)
https://www.youtube.com/watch?v=ErmOTERAnQo
The Pain Revolution Website
The Pain Revolution resources page
www.painrevolution.org/newresources
Four Essential Pain Facts
www.painrevolution.org/painfacts
Endnotes
1. For more information about the International Association for the Study of Pain, see their website at https://www.iasp-pain.org/. In 2020, IASP revised its definition of pain: “Pain is always a personal experience influenced to varying degrees by biological, psychological, and social factors. Pain and nociception are different phenomena. Pain cannot be inferred solely from activity in sensory neurons. Through their life experiences, individuals learn the concept of pain. A person’s report of an experience as pain should be respected. Although pain usually serves an adaptive role, it may have adverse effects on function and social and psychological well-being. Verbal description is only one of several behaviors to express pain; inability to communicate does not negate the possibility that a human or a nonhuman animal experiences pain” (International Association for the Study of Pain 2024, online).
2. The gate control theory of pain suggests that pain perception is regulated by a complex interaction of signals within the nervous system (Campbell, Johnson, and Zernike 2020; Sufka and Price 2002; Melzack 1996). The spinal cord functions as a gatekeeper, either permitting or blocking pain signals that travel along small nerve fibers to the brain. Larger nerve fibers carrying non-painful sensations, like touch, can close this gate and inhibit pain signals. Furthermore, the brain can affect this gating mechanism, with psychological factors such as attention, expectations, and emotions either opening or closing the gate, thus modifying the pain experience. This theory highlights that pain is not simply a direct sensory response but also involves significant psychological and emotional factors, which explains why individuals experience pain differently. In chronic pain, this gating mechanism may become dysfunctional, leading to a heightened sensitivity to pain or the perception of pain without any obvious physical cause. This can result in persistent pain even after the original injury has healed, emphasizing the need for treatments that address both the physical and psychological components of pain.
3. The biopsychosocial model was introduced by George Engel in a seminal paper titled “The Need for a New Medical Model: A Challenge for Biomedicine,” which was published in the journal Science in 1977. This model offers a framework for understanding health and illness through the integration of biological, psychological, and social/cultural factors, and is particularly relevant in the context of chronic pain (Lugg 2022). Biological factors in chronic pain include genetic predispositions, neurochemical imbalances, chronic inflammation, nerve damage, maladaptive pain pathways, and ongoing infections or illnesses. Psychological factors in chronic pain include anxiety, depression, negative thoughts, avoidance behaviours, muscle deconditioning, and ineffective coping strategies can all amplify and perpetuate the perception of pain. Social factors in chronic pain include limited access to healthcare, financial stress, cultural attitudes, family dynamics, social support networks,
and environmental and societal norms, all of which can influence the experience and management of pain. Cultural differences significantly influence how chronic pain is perceived, expressed, and managed across different societies. These differences encompass attitudes toward pain, beliefs about its causes and consequences, and cultural norms regarding pain expression and treatment-seeking behavior. For example, some cultures may view pain as a natural part of life and prioritize stoicism and endurance, while others may encourage more open expression of pain and seek immediate medical intervention.
4. The process where nociceptive input does not create the experience of pain is called nociceptive
modulation or, more specifically, descending
inhibition (Apkarian 2019; McKune et al. 2015). This process involves the brain and spinal cord mechanisms that can suppress or modulate pain signals before they reach conscious awareness. In this context, the nervous system regulates and sometimes inhibits nociceptive input to prevent it from being perceived as pain; it is like turning the volume knob down on nociceptive signaling. This can happen through various mechanisms, such as the release of endogenous opioids (such as endorphins and enkephalins) or the activation of certain neural pathways that dampen the pain signals, such as the dorsolateral funiculus, a spinal pathway that carries the descending inhibitory signals from the brain stem to the dorsal horn of the spinal cord, where they can inhibit nociceptive transmission (Latremoliere and Woolf 2009; Harte, Harris and Clauw 2018; Woolf 2019).
5. According to Andy Clark (2023, xii): “Contrary to the standard belief that our senses are a kind of passive window onto the world, what is emerging is a picture of an ever-active brain that is always striving to predict what the world might currently have to offer. Those predictions then structure and shape the whole of human experience, from the way we interpret a person’s facial expression, to our feelings of pain, to our plans for an outing to the cinema. Nothing we do or experience – if the theory is on track – is untouched by our own expectations. Instead, there is a constant give-and-take in which what we experience reflects not just what the world is currently telling us, but what we – consciously or unconsciously – were expecting it to be telling us. One consequence of this is that we are never simply seeing what’s ‘really there,’ stripped bare of our own anticipations or insulated from our own past experiences. Instead, all human experience is part phantom – the product of deep-set predictions. We can no more experience the world ‘prediction and expectation free’ than we could surf without a wave.”
6. Smudging of body maps refers to changes in the brain’s representation of the body, particularly in the primary somatosensory cortex (Hargrove 2019). Smudging is also called cortical remapping or cortical reorganization. The primary somatosensory cortex contains a somatotopic map, known as the homunculus. This map spatially organizes different parts of the body, with specific regions of the cortex corresponding to distinct body parts. Chronic pain can cause an altered sensory representation where the specific areas of the brain that represent particular body parts can become less distinct and more diffuse. There can also be changes in neuronal activity in the somatosensory cortex, where neurons that previously responded to stimuli from a specific body part may start responding to stimuli from a broader area or even from different body parts.
Alan Richardson is a Certified Advanced Rolfer™ and Rolf Movement® Practitioner with a private practice in London, UK since 1998. He is also qualified as a craniosacral therapist. Richardson is passionate about knowing other cultures and languages, having lived in Japan, Taiwan, Australia, and Brazil.
References
Apkarian, Apkar Vania. 2019. Definitions of nociception, pain, and chronic pain with implications regarding science and society. Neuroscience Letters 702:1-2.
Brinjikji, W., P. H. Luetmer, B. Comstock, B. W. Bresnahan, L. E. Chen, R. A. Deyo, S. Halabi, J. A. Turner, A. L. Avins, K. James, J. T. Wald, D. F. Kallmes, and J. G. Jarvik. 2015. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. American Journal of Neuroradiology 36(4):811-816.
Bryson, Bill. 2019. The body: A guide for occupants. London, United Kingdom: Doubleday.
Butler, David S., and G. Lorimer Moseley. 2013. Explain pain, second edition. Adelaide, Australia: Noigroup Publications.
Campbell, Travis S., Jillian A. Johnson, and Kristin A. Zernicke. 2020. Gate control theory of pain. In Encyclopedia of Behavioral Medicine M. D. Gellman (Ed.), 914-916.
Chatterjee, Rangan. 2022. How to heal chronic pain with Dr. Howard Shubiner. Episode 310. Available from https://podcasts.apple.com/gb/podcast/310-how-to-heal-chronic-pain-with-dr-howard-schubiner/id1333552422?i=1000585376328.
Clark, Andy. 2023. The experience machine: How our minds predict and shape reality. London, United Kingdom: Penguin.
Doidge, Norman. 2007. The brain that changes itself. New York: The Penguin Group.
Engel, George. 1977. The need for a new medical model: A challenge for biomedicine. Science 196:129-136.
Frankl, Viktor E. 1959. Man’s searc for meaning. Boston, Massachusetts: Beacon Press.
Hargrove, Todd. 2019. Playing with movements: How to explore the many dimensions of physical health and performance. Seattle, Washington: Better Movement.
Harte, Steven E., Richard E. Harris, and Daniel J. Clauw. 2018. The neurobiology of central sensitization. Journal of Applied Biobehavioral Research 23:e12137.
Hebb, Donald O. 1949. The organization of behavior. New York: Wiley and Sons.
International Association for the Study of Pain. 2020. IASP announces revised definition of pain. Available from https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/. Accessed November 27, 2024.
Kragel, Philip A., Leonie Koban, Lisa Feldman Barrett, and Tor D. Wager. 2018. Representation, pattern information, and brain signatures: From neurons to neuroimaging. Neuron 99(2):P257-273.
Latremoliere, Alban, and Clifford J. Woolf. 2009. Central Sensitization: A generator of pain hypersensitivity by central neural plasticity. The Journal of Pain 10(9):895-926.
Lugg, William. 2022. The biopsychosocial model – history, controversy and Engle. Australasian Psychiatry 30(1):55-59.
Lyman, Monte. 2021. The painful truth. London, United Kingdom: Bantam Press.
Luchau, Til, and Whitney Lowe. 2022. Episode 111. The Thinking Practitioner Podcast. Available from www.youtube.com/watch?v=JZhf0QNassE.
McKechnie, Grant. 2022. Webinar: Introduction to the essential pain facts pain revolution. Available from https://www.youtube.com/watch?v=5ga8CRAqGkk.
McKune, Carolyn M., Joanna C. Murrell, Andrea M. Nolan, Kate L. White, and Bonnie D. Wright. 2015. Nociception and pain. In Veterinary Anesthesia and Analgesia: The fifth edition of Lumb and Jones. New York: John Wiley and Sons, Inc.
Melzack, Ronald. 1996. Gate control theory: On the evolution of pain concepts. Pain Forum. 5(1):128-138.
Melzack, Ronald, and Patrick D. Wall. 1965. Pain mechanisms: A new theory. Science 150:971-979.
Moseley, G. Lorimer. 2011. Why things hurt. Available on YouTube at https://www.youtube.com/watch?v=gwd-wLdIHjs&t=89s.
O’Malley, Callum A., Samuel A. Smith, Alexis R. Mauger, Ryan Norbury. 2024. Exercise-induced pain within endurance exercise settings: Definitions, measurement, mechanisms and potential interventions. Experimental Physiology 109:1446-1460.
Pain Revolution. 2024. Pain facts. Available from www.painrevolution.org/painfacts. Accessed November 27, 2024.
Purves, D., G. J. Augustine, D. Fitzpatrick, et al. (Eds.) 2001. Nociceptors. In Neuroscience. 2nd edition. Sunderland, Massachusetts: Sinauer Associates.
Ramachandran, V. S. and Sandra Blakeslee. 1998. Phantoms in the brain: Probing the mysteries of the human mind. London, United Kingdom: William Morrow.
Richardson, Alan. 2024. Rolfing Holism. Structure, Function, Integration 52(1):106-111.
Rolf, I.P. 1989. Rolfing: Reestablishing the natural alignment and structural integration of the human body for vitality and well-being. Rochester, Vermont: Healing Arts Press.
Sizer, Phil. 2019. Chronic pain the drug-free way. London, United Kingdom: Sheldon Press.
Schubiner, Howard, and Michael Betzold. 2019. Unlearn your pain: A 28-day process to reprogram your brain. Pleasant Ridge, Michigan: Mind Body Publishing.
Sperry, Roger Wolcott. 1981. Changing priorities. Annual Review of Neuroscience 4:1-15.
Sufka, Kenneth J., and Donald D. Price. 2002. Gate control theory reconsidered. Brain and Mind. 3:277-290.
Van der Kolk, Bessel. 2014. The body keeps the score: Brain, mind, and body in the healing of trauma. London, United Kingdom: Allen Lane.
Woolf, Clifford J. 2011. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 152:S2-S15.
Woolf, Clifford J. 1983. Evidence for a central component of postinjury pain hypersensitivity. Nature 306:686-688.
Young, Emma. 2021. Super senses: The science of your 32 senses and how to use them. London, United Kingdom: John Murray.
Keywords
pain; acute pain; chronic pain; nociception; gate control theory; Rolfing Structural Integration; neuroplasticity; central sensitization; biopsychosocial model; pain education; sensorimotor maps; graded exposure; therapeutic relationship; counterirritation. ■
View all articles: Articles home



