ABSTRACT At the 7th Fascia Research Congress in New Orleans, Louisiana, Dr. Carla Stecco shared her enthusiasm about the growing global collaboration and scientific rigor in fascia research. Stecco discusses her keynote on lipedema, revealing that affected individuals have thicker, more collagen-rich superficial fascia and larger, poorly supported adipose lobules. Also, Stecco suggested that precise knowledge of which fascial layers are affected by fascial pathology can help practitioners choose the most appropriate manual techniques.
Editor’s note: This conversation took place in person on August 14th, 2025, at the 7th Fascia Research Congress at the Marriott Hotel in New Orleans, Louisiana. The four-day conference drew approximately 600 attendees, with Dr. Carla Stecco serving as one of the keynote speakers.
Connecting Fascia Researchers and Practitioners
Lina Amy Hack: We are here in New Orleans, Louisiana, for the 7th Fascia Research Congress (FRC) with Dr. Carla Stecco (see Figure 1). Thank you for meeting to discuss fascia research and your thoughts on fascia science. How has your experience been this week? What impressions stand out for you?
Carla Stecco: Thank you, Lina. I’m very happy because I saw people enthusiastic and looking for new connections to further their fascia research. All the people here at the conference have brought their knowledge, and they are also discovering new knowledge that others have shared. This is a unique feeling that we can have together in our congress. There is a lot of fun happening. I am finding that people really love this topic, and they want to connect with me about it, and that is amazing to me; so much joyful interest in fascia.
Also, I have felt happy because there has been very good research presented. I think that fascia research is moving to the next level of knowledge because we have started to have many different research groups from around the world that are looking at fascia in a scientific way. Some are demonstrating qualities about different fascia-related cells, new information about the innervation of fascia, and others are developing ultrasound techniques to ask new questions about fascia. It’s all very good.
Lina: That is so true. Great research is being presented, and meaningful connections are being made between the talks. People seem very interested in engaging with new individuals, one-on-one and in small groups, which is
so rewarding.
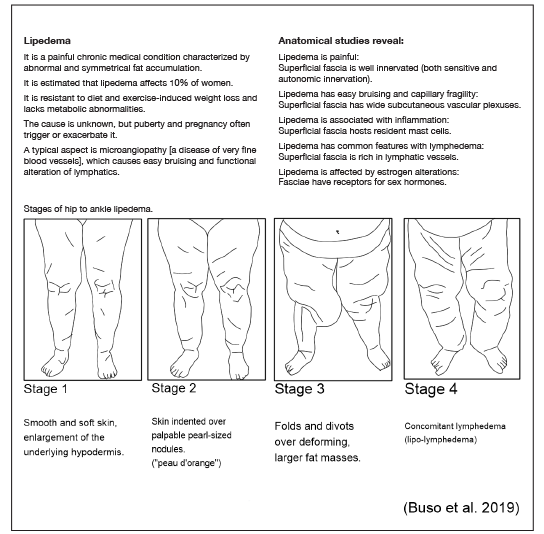
You delivered a keynote presentation on Monday morning titled, “Role of Fascial Alterations in Lipedema.” And your talk focused on the superficial fascia of people with lipedema (see Figure 2). As a Rolfer®, I have had many clients over the years who present with this body condition. One part of your work that stayed in my mind was that you demonstrated that, for people with lipedema, the superficial fascia at the hip is thicker, has more collagen, a thicker retinacula cutis, and has larger fat lobules that are not well-supported by the retinacula cutis.
For Rolfers, we often work with our clients side-lying, and your talk had me thinking about the time I’ve spent doing compression and shearing work with this kind of tissue. I know what you mean when you described the lumpy nodules. The tissue needs special consideration; it could bruise easily, it seems inflamed, and the person may experience touch interventions as painful.
Carla Stecco: I think that fascia research is moving to the next level of knowledge because we have started to have many different research groups from around the world that are looking at fascia in a scientific way.
Anecdotally, I’ve had success with these clients; they tell me the Rolfing Ten Series® seemed to diminish their generalized experience of pain and increase their experience of comfort in their bodies.
Would you hypothesize that direct manual therapy targeting the superficial fascia in individuals with lipedema is addressing this tissue? Would you think that the fascia may become more organized with manual input?
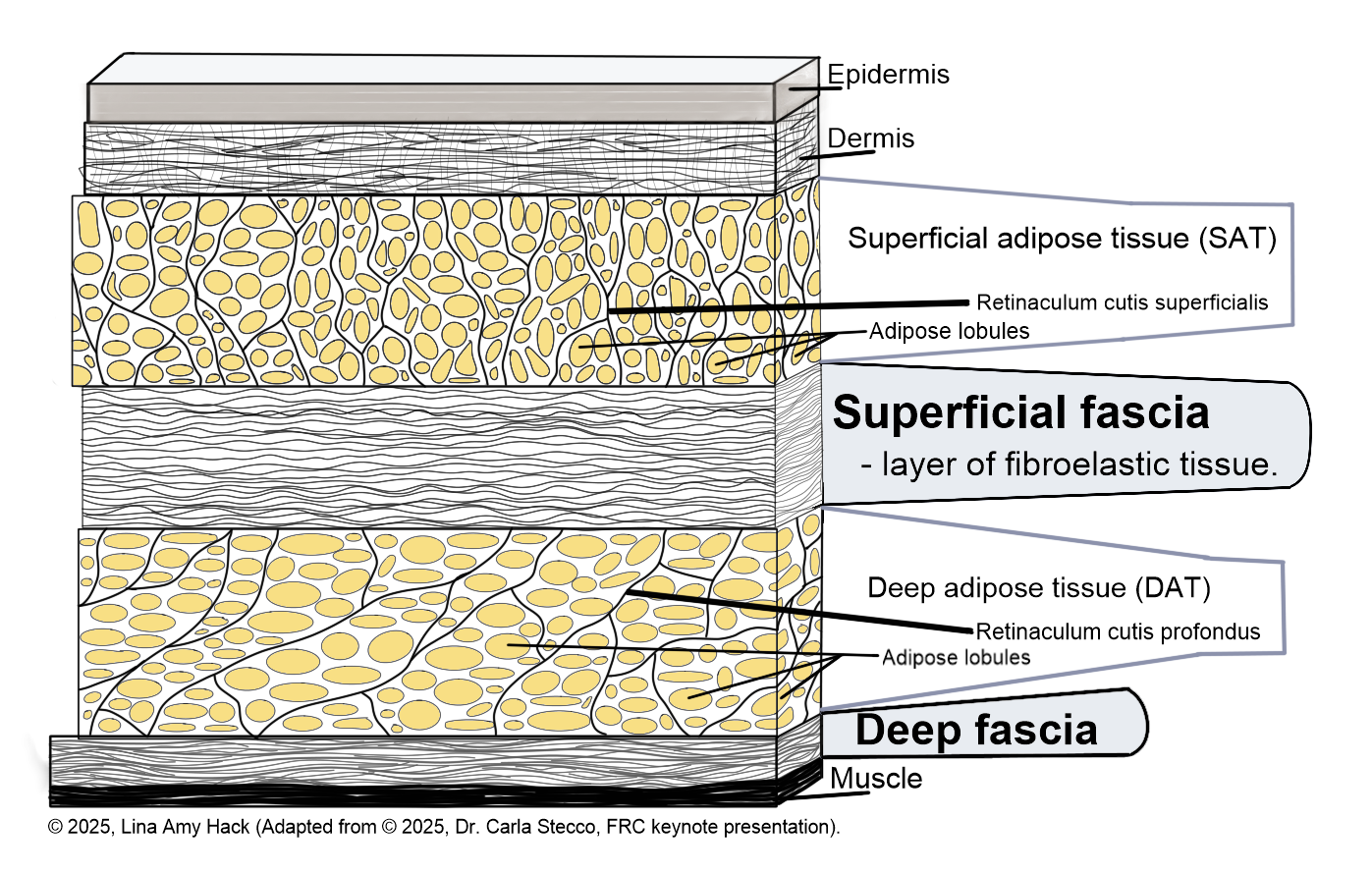
Carla: I think so. The better knowledge we have of what fascia is involved, then we know what tissue is involved with the person’s discomfort, and this can allow us to be more precise in the manual technique we apply and also in the selection of the modality of the approach. Lipedema seems to be a pathology that is affecting the superficial fascia and what they call the deep deposition, which is the interface between the superficial fascia and the deep fascia. (See figure 3.) So, we need to focus on the mobilization of that part.
We know that in the lipedema patient, there is also inflammation, acute and chronic, and consequently probably we need to pay attention to not be too aggressive because they already have inflammation. So, we need to stimulate a better movement of the superficial fascia with respect to the deep fascia without stimulating the inflammation.
As a Fascia Manipulation® teacher, I’m not afraid of the inflammation because in the deep fascia, we are looking for the inflammation to stimulate the remodeling. But in this type of patient, I think that at least at the beginning, we need to silence the immunity component and not trigger too much inflammation.
Lina: Makes sense. The histology images that you presented showed that this fascia is more disorganized. Maybe this is a simple way to think about it, but do you think that there is an ideal manual therapy pressure and direction of force into these layers that may assist in the fascia becoming more organized?
Carla: Yes, I expect that. If we are able to restore mobilization between the superficial fascia and the deep fascia, the mechanical line of force may assist in the remodeling of the superficial fascia. Remember, all the time our superficial fascia is under remodeling, but if we have some adhesion, the remodeling is not going well. So we need to free the tissue, to restore the gliding, and that way the remodeling can work much better.
Paying Attention to Hyaluronan
Lina: Fascinating. You also reported the observation that the superficial fascia of lipedema patients has an increase of hyaluronan (also known as HA) and water, giving the lipedema adipose a stiffer quality. Also, HA can be linked to the induction of pro-inflammatory events. That’s very interesting because I usually think about HA as a molecule that allows for the slide and glide between fascial layers.
Carla: Hyaluronan has an incredible spectrum of functions. Depending on the molecular weight of the HA in the tissue, it could be pro-inflammatory or it could be anti-inflammatory. In some conditions, HA stimulates new vascularization, but in other conditions, HA can stop the vascularization. So, we are not sure what can cause the hyaluronan in lipedema patients to be stiff because we don’t know the molecular weight of the hyaluronan that is produced for them specifically. But what it could be, we are sure that in the sample we found other cytokines such as the TNF-alpha, some metabolic lipids related with the inflammation that really suggests that we have an HA molecule associated with the inflammation inside the superficial fascia.
Lina: Your description leads me to think that HA is more a family of molecules, not just a singular molecule.
Carla: The molecule is always the same, but it can aggregate, and other chemical groups can be added on, changing its molecular weight. HA can be found as very small molecules that are just a few kilodalton’s of weight, and there are also HA aggregates of 2,000 kilodaltons. Consequently, there is a really huge spectrum in size of hyaluronan, and different functions of the different sizes.
Lina: That is fascinating because hyaluronic acid is a buzzword in society now. I see it on cosmetic packaging; health products claim their products contain it, but your presentation got me thinking that it isn’t just a singular molecule. It is more dynamic than that in the body, and we have to learn more about it.
Carla: Yes, absolutely. Also, in the media, hyaluronan is spoken of as something that is always good, but that is probably not exactly how we should think of it. People have started to inject hyaluronan inside the fascia, but what is the molecular weight that they are injecting? We don’t need high molecular weight, most likely, as we do inside the joint, because we need something that is smaller, that allows gliding. We don’t want something that creates resistance to the compression. So, yes, we need to pay more attention to this molecule.
Lina: Would you hypothesize that direct manual therapy targeting the superficial fascia in individuals with lipedema is addressing this tissue? Would you think that the fascia may become more organized with manual input?
Carla: I think so. The better knowledge we have of what fascia is involved, then we know what tissue is involved with the person’s discomfort, and this can allow us to be more precise in the manual technique we apply and also in the selection of the modality of the approach.
Lina: I would think people need to be cautious about the source of the HA that they’re injecting.
Carla: And that is another key problem, not only for the source of that external hyaluronan, but also who produced that product. We need to think about what are the correct inputs to stimulate inside the body for the production of our own hyaluronan.
Lina: This was one of my key takeaway messages from your talk. It painted a sophisticated picture about that molecule and that we shouldn’t reduce it down to being just one thing.
Carla: Exactly.
Carla: Hyaluronan has an incredible spectrum of functions. Depending on the molecular weight of the HA in the tissue, it could be pro-inflammatory or it could be anti-inflammatory.
Including the Interstitium
Lina: In January 2025, you and a team of fascia researchers published the paper, “Towards a Comprehensive Definition of the Human Fascial System” (Stecco et al. 2025). Can you tell us about the fascial interstitium? And is it always associated with the collagen-elastin matrix?
Carla: In this new definition, we tried to find a comprehensive definition that captures the microscopic nature of fascia to the macroscopic. Fascia is not only a layer that we can work with our hands, and dissect, but fascia is also the element that allows transmission of the force and creates a gliding interface that allows movement at the molecular level. And the interstitium is exactly the smallest; this definition includes the very small microscopic part of the fascia.
At the microscopic level, that is where we have the fluid that moves, this is where we have the gliding between different cellular structures, between the vessels and the surrounding tissue, between the small nerve and the surrounding tissue. So, I think we can include the interstitium in the definition of fascia, considering this very broad vision that moves from the macroscopic level to the microscopic.
Lina: That’s exciting to hear. In the structural integration profession, we feel and listen to all the different fascial layers you and your colleagues describe. We will sometimes feel significant textural changes while working, where the tissue starts out stiff and firm, then becomes soft and pliable within minutes of our manual interventions. What do you think can account for these palpatory changes that manual therapists experience?
Carla: I think that is the hyaluronan and the water component that can modify easily because the fibrotic component, the collagen and elastin, can only be modified by remodeling. If manual interventions do free their tissue, if we recreate the gliding that is possible, then we can also improve the collagen fiber. But it’s not a direct work of the manual treatment because fascia is much too stable to have modifications with just forces applied by hand.
The water component and the hyaluronan can easily be modified with the manual treatment. So, when we are stiff, it’s like we expect that it is like a concentration of hyaluronan, an aggregation of hyaluronan that links water and creates a stiffer tissue. By applying manual forces, maybe we move the big water-bound molecules to become smaller aggregations, and we recreate the gliding.
We also trigger some inflammation, and that can trigger the remodeling of the fibrotic component. And it is for that reason that I think that manual treatment is a key element to start the process. When thinking about how to fix chronic issues in the fascia, manual therapy and adding some exercise along the direction where we have broken the fixations and stimulate the correct alignment of the collagen fiber production.
The Work Continues After the Session
Lina: Ida Rolf [PhD, (1896-1979)] was known for saying to her students that the changes induced by manual fascial work happen after the client has left the session; the change happens after they leave the office. Your research seems to correlate with that observation, that the forces of manual therapy begin fascial remodelling that progresses for hours after the intervention. Is this true?
Carla: Yes, I totally agree with Rolf because I think that we just trigger a process, but we are not really able to modify fascia directly or in a stable way. The situation is, the body can stabilize the result of the input. And it’s for this reason that finding the correct equilibrium in the point treated is important because otherwise, the patient comes back later.
Fascia Research at Health Conferences
Lina: These are the kinds of things being talked about at the FRC and it is both practitioners and researchers talking about two sides of the same fascia coin, so to speak. I’ve been wondering as I listen to everybody: doesn’t fascia research also belong at other health and medical conferences?
Carla: I am sure that the information about the human fascia system needs to be brought to other conferences, but it’s not as easy as you might think. Last year, I attended the World Congress of Pain, a conference held in Amsterdam, Netherlands, in August 2024. Professor Helene M. Langevin, director of the National Center for Complementary and Integrative Health (NCCIH), was with me, and together we were a pretty strong team.
Lina: Wow, you two are among our ‘heavy hitters’ in fascia research. How’d it go?
Carla: We were the only two people who spoke about fascia in the entire conference. It was disappointing because the conference was huge, with about 5,000 people in attendance, and nobody else spoke about fascia and pain. So, here we are at the fascia conference; we think that everyone knows about fascia. But it’s not true. We have a lot of work to do to attract other medical and health professionals to be interested in what we know. And, it’s the same with other conferences as well; there is a lot of work to do to let other professionals know about fascia research.
Lina: We have a big mountain to climb for fascia health to be considered important by general healthcare practitioners.
Carla: Exactly. And it is for that reason that I stress the concept of terminology in my publications because if we are not clear in the definition of what is fascia, why fascia is important, and what are the key elements that we need to explain this to professionals outside this circle here, then it would be very difficult to communicate with other people.
One profession that is curious about fascia is the anesthesiologists because they use the fascial planes to treat pain when patients need an anesthetic block. So they are a little more open-minded. We are starting to gain the interest of plastic surgeons, but there is still an incredible amount of work that needs to be done.
Lina: We have a big mountain to climb for fascia health to be considered important by general healthcare practitioners.
Carla: Exactly. And it is for that reason that I stress the concept of terminology in my publications because if we are not clear in the definition of what is fascia, why fascia is important, and what are the key elements that we need to explain this to professionals outside this circle here, then it would be very difficult to communicate with other people.
Lina: My sister is a family doctor in Canada and she’s often going to conferences. I think there’s probably no fascia research being talked about at those conferences – and there needs to be! I think there would be a place for it at any one of these medical topics that doctors are invested in.
Carla: Absolutely. I was asked to share fascia topics with a conference about the voice, they asked me to give a lecture about fascia. And I am happy to go there because it’s like a window of opportunity has opened, to talk to this different group. But really, we are at the beginning.
Teaching Fascial System in Medical Schools
Lina: And last time we spoke in 2022, you mentioned the challenge it is to get fascia known and taught in medical schools. How is that line of education going? Are we still at the beginning of getting this information taught to future doctors?
Carla: It is going better in respect to last time. Two months ago, I was at the Congress of the American Anatomists, and I spoke to them in a session about fascia. I spoke about how important it is to teach the anatomy of fascia to students. And at the end of the session, one professor said, “Okay, we are convinced that we need to speak to our students about fascia. Now we just need to understand what are the ways to teach this information, in which course does fascia belong, and what are the key concepts that we need to transmit in the limited time we have with the students.”
So I think this is good, now they have an interest in fascia and fascia research. Now, other feedback is needed to introduce this topic. From our side with our Fascia Research Society, we need to understand what has to be taught and in what way because they are now asking us about that problem.
Lina: That’s great news! Thank you so much for doing this hard work in fascia research and communicating to the medical and health world about the human fascial system. I think our beloved Dr. Rolf would have loved talking with you and listening to your presentations. She certainly would have invited you into her parlour for coffee and tea many times to discuss all of this at great length. You are doing some heavy intellectual lifting for all manual therapists, and we are all here to support you. I see this with my own eyes here at this conference: so many talented movement and manual therapists mingling with the researchers. As a group, we value you. You are substantiating what we claim we are doing in our treatment rooms. Because of you, we bring to our clients scientific knowledge of what fascia is and how it responds to our work. Thank you for your time today, it is wonderful to see you in person.
Carla: You are welcome, Lina.
Dr. Carla Stecco is an orthopedic surgeon and professor of human anatomy and movement sciences at the University of Padova, Italy. She is a founding member of the Fascial Manipulation Association and of the Fascia Research Society. Her scientific activity is devoted to the study of the anatomy of human fasciae from a macroscopic, histological, and physio-pathological point of view. She has personally done over a hundred human cadaver dissections for research. She is the author of several books and more than a hundred and eighty peer-reviewed articles.
Lina Amy Hack, BS, BA, SEP, became a Rolfer® in 2004 and is now a Certified Advanced Rolfer (2016) practicing in Canada. She has an honors biochemistry degree from Simon Fraser University (2000) and a high-honors psychology degree from the University of Saskatchewan (2013), as well as a Somatic Experiencing® Practitioner (2015) certification. Hack is the Editor-in-Chief of Structure, Function, Integration
References
Buso, Giacomo, Michele Depairon, Didier Tomson, Wassim Roffoul, Roberto Vettor, and Lucia Mazzolai. 2019. Lipedema: A call to action! Obesity 27:1567-1576.
Stecco, Carla, Rebecca Pratt, Laurice D. Nemetz, Robert Schleip, Antonio Stecco, and Neil D. Theise. 2025. Towards a comprehensive definition of the human fascial system. Journal of Anatomy 00:1-15.
Keywords
Fascia Research Congress; superficial fascia; lipedema; retinacula cutis; Rolfers; Fascia Manipulation; deep fascia; inflammation; hyaluronan; fascial interstitium; human fascial system. ■
View all articles: Articles home



