ABSTRACT This article discusses dural tube adhesions, their causes, and a manual therapy point of view for their release. Author, Certified Advanced Rolfer™, and continuing education instructor Jeffrey Burch explores how adhesions form due to trauma (for example, whiplash) or infection (for example, meningitis), and how they may restrict spinal movement, leading to discomfort. Burch describes a manual intervention method that involves palpating vertebrae to assess the dural tube restrictions and then applying specific techniques to restore glide within the dural tube. He emphasizes precision and caution when working with the dural tube of your client.
Dural Tube Adhesion Release Method Assessment and Treatment
As Rolfers™, structural integration practitioners, and manual therapists, one of the fascial manipulations we deploy is to locate adhesions between the dural tube and the periosteum of the neural canal. This particular focus deserves caution because of the delicate nature of these tissues. Yet, with study and care, we can palpate through vertebral spaces and restore glide to those areas. The method is the same for all the thoracic and lumbar vertebrae; a somewhat different variation of this method is used with the neck. In addition, the upper cervical vertebrae C1, C2, and C3 have a distinctly different relationship to the dural tube than C4 to C7. Assessing and treating each of these sectors of the dural tube is explained below.
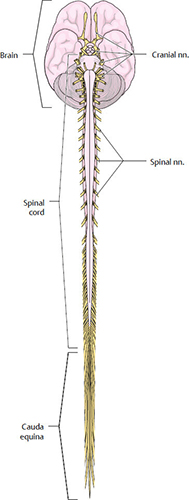
The dural tube is the outermost of three concentric tubular layers of connective tissue membrane surrounding the spinal cord inside the neural canal (Kekere and Alsayouri 2023). It has natural attachments to the full perimeter of the foramen magnum, the entire circumference of C1 and C2, and highly variable portions of C3.
Following any injury to any portion of the dural tube, the fibroblasts, a migratory cell type, will work to repair the injured connective tissue. There are two common ways by which the dural tube is injured: whiplash and infection.
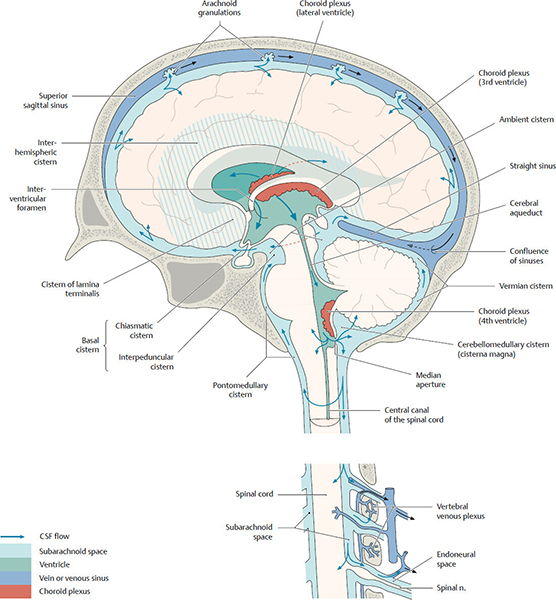
At its inferior end, after all of the nerves have departed from the meninges, the now empty tubes condense to form a cord called the filum terminale, which attaches posteriorly to the first coccygeal segment. Superior to that, within the sacrum, the dural tube attaches to the body of the second or third sacral segment (Ünal and Sezgin 2021). Rarely the inferior attachment of the sural tube is on the anterior surface of the body of the fifth lumbar vertebra rather than to a sacral segment. Normally, the dural tube glides through all other vertebrae when the axial complex moves dynamically. This glide is important for good spinal movement and comfort.
Following any injury to any portion of the dural tube, the fibroblasts, a migratory cell type, will work to repair the injured connective tissue. Fibroblasts are cells that remove damaged collagen and elastin fibers and produce new connective tissue fibers to restore the structural integrity of damaged tissue, including the dural tube. Fibroblasts are migratory, swimming through the interstitial spaces of our body. Normally, the new fiber produced by the fibroblasts is woven into the structure of the connective tissue being repaired, in this case, the dural tube. Sometimes, portions of this new fiber are also laid down across lubricated gliding surfaces, like between the dural tube and the nearby periosteum on the bony surfaces of the neural canal through the vertebrae. The more severe the injury to the dural tube, the more likely such adhesions are to form.
If the whole length of the spinal dura, occiput through the sacrum, becomes infected, the dural tube will form adhesions to the periosteum of most or all of the vertebrae, producing lasting stiffness and back pain.
Whiplash:
The dural tube has limited elasticity. It can only stretch about five percent of its length. Because the dural tube is anchored to the foramen magnum, when the head is ballistically accelerated, the pull on the dural tube from the cranium snapping forward or backward will instantaneously use up the stretch in the dural tube. Then, as the head continues to move quickly, the dural tube can become injured. If the dural tube is torn through, this serious injury requires a surgical repair. Short of a full tear, the sharp pull of whiplash can injure the dural tube, fraying it but not tearing through and through.
Infection:
Three concentric tubular membranes surround the spinal cord. Think of wearing three layers of socks on a cold day. The tough dura is the outermost of these three layers. Next comes the softer arachnoid layer. Deep to the arachnoid membrane, closest to the spinal cord, is also the soft pia mater. Think of these three together on the inner surface of vertebrae, like cushioned bubble wrap inside a cardboard box; together, they protect the contents, the rather fragile spinal cord. The dura, arachnoid, and pia membranes are collectively known as the meninges.
If the meninges membranes become infected, the condition is called meningitis. Several different microbes may infect the meninges. Meningitis is often but not always a severe condition that can result in permanent disability or death.
If the whole length of the spinal dura, occiput through the sacrum, becomes infected, the dural tube will form adhesions to the periosteum of most or all of the vertebrae, producing lasting stiffness and back pain. Fortunately, most cases of spinal meningitis affect only a local area of the meninges before the immune system kills the microbes. More serious cases of meningitis will be diagnosed and treated medically. The ‘subclinical’ cases often never come to medical attention. We associate meningitis with young people in congregate settings such as dormitories or barracks. More mature people rarely get meningitis because they had a subclinical case in their youth and then have lifetime immunity.
In a subclinical case of meningitis, the person will be aware of having a brief flu-like illness with some back muscle pain. This focal meningitis will produce one or more focal adhesions at the site or sites of infection.
To assess these possibilities, have the client in a side-lying position. Put a pillow in front of their torso for them to drape their arm over. . . . With your right hand, engage the bone of the sacrum and draw it inferior. Be sure to engage the bone, not just the skin overlying the sacrum. As you pull the sacrum inferior, feel how the vertebrae under your left hand and forearm move.
Manual Intervention with the Dural Tube
To visualize the assessment and treatment process for dural tube adhesions, it is helpful to think of each vertebra, viewed from the side, as a little teeter-totter with the fulcrum at the facet joints. If the spinous process of a single vertebra is moved superior on this pivot, the body of the vertebra tips inferior and vice versa.
Since the dural tube is attached to the sacrum, if the sacrum is pulled inferiorly, the spine will lengthen, and if there are no dural tube adhesions, the row of spinous processes will fan open wider in a linear way in response to this pull. But if the dural tube is adhered to a vertebra, that vertebra will move differently than its neighbors when the sacrum is pulled inferiorly. The direction the spinous process will move when offering sacrum traction depends on where in the neural canal the dural tube adhesion is located. If the dural tube has adhered to the periosteum in the posterior half of the neural canal, then the posterior part of the vertebra will be pulled inferiorly faster than the neighboring vertebrae. On the other hand, if the dural tube adhesion is anterior in the neural canal, the spinous process will teeter-totter around the facet joints and go superior while its neighbors are moving inferior.
To assess these possibilities, have the client in a side-lying position. Put a pillow in front of their torso for them to drape their arm over. This provides some stability, so you can push into their back without their having to use muscular effort to prevent themselves from rolling forward. If the person is lying on their left side, place the ulnar edge of your left hand and forearm on their spinous processes, with the tip of your 5th finger at L5. With your right hand, engage the bone of the sacrum and draw it inferior. Be sure to engage the bone, not just the skin overlying the sacrum. As you pull the sacrum inferior, feel how the vertebrae under your left hand and forearm move. Do the spinous processes all fan open evenly, or did any of the spinous processes move inferior faster than the neighboring vertebrae? Or did any spinous processes move superior while its neighbors all go inferior? You will feel the spinous process movement as you pull the sacrum inferior. There is nothing to feel once the sacrum is in an inferior position, the movement is over. You have to catch it on the fly.
If you felt a vertebra that moved differently than its neighbors, first relax your traction on the sacrum, then move your left hand to contact that vertebra of interest with your fingers in a way that you can control that vertebra. Now, with your sacral hand, once again, draw the sacrum inferior. With the fingers of your vertebral hand, prevent that vertebra from making the aberrant movement it did before. If its spinous process went down faster than its neighbors, provide support from below (inferiorly), so it can’t go inferior as you again pull down on the sacrum. Now, gently pull down on the sacrum, just enough so there is a first barrier load between your two hands. This sets up a first barrier shear through the dural tube adhesion within the vertebra you are holding.
The adhesion may be squarely posterior in the dural tube or more to one side, in either the right or left posterior quadrant. While you have the first barrier shear load along the dural tube established, with that tension between the sacrum and the vertebra, slowly rotate the spinous process of the vertebra around an anterior-posterior axis, first clockwise and then counterclockwise. If the tension between your hands decreases while rotating one way and increases while rotating the other way, this tells you the adhesion is more to one side, though still mainly in the posterior part of the neural canal. Use this rotary component to adjust your load on the vertebra more precisely with respect to the location of the dural tube adhesion.
After you feel a release between your hands, slack the pull on the sacrum and lessen the load on the vertebra. Recheck by pulling the sacrum down while monitoring that vertebra. You may now find an adhesion in a different sector of the neural canal of that vertebra. If so, use the same analytic process to figure out where the remaining adhesion is and set up a first barrier shear to release it. Repeat this cycle until this vertebra no longer moves differently than its neighbors when you pull inferior on the sacrum.
Remember to keep an open mind about the many possibilities of adhesions. The dural tube adhesion can be in any part of the neural canal. It can be narrow or broad, up to the full circumference of the tube. Two or more separate adhesions may exist in different parts of the neural canal at the same vertebra.
If the dural tube adhesion is full circumference, the spinous process will initially behave as it does for a posterior dural tube adhesion, which is descending toward the sacrum faster than its neighbors as you traction the sacrum. Initial treatment will release the posterior portions of the full circumference adhesion. Then, when you re-test, the spinous process will ascend rather than descend. Now, you can treat the anterior portion.
Most people have more than one dural tube adhesion. Most people have had more than one head snap; it is paying for the big brain on the end of a narrow stalk. Many people have had a subclinical case of meningitis. The process described here will usually, but not always, show you the adhesion closest to your fractioning hand first. After the first adhesion found is released, you can see the next one along the spine, and so forth.
This process works well for lumbar and lower thoracic vertebrae. Instead of pulling down on the sacrum, you can pull up on the occiput. This is more useful for upper thoracic vertebrae, although you may feel it down in the lumbar vertebrae. Make sure the pull on the occiput is straight, linear, and superior; do not flex or extend the neck. When you pull on the occiput, the movement of the spinous processes follows the same principles, but the direction of movement will be the opposite. If the dural tube adhesion is posterior in the neural canal, the spinous process will follow the occiput superior faster than its neighbors. If the dural tube adhesion is anterior in the neural canal, the spinous process will move inferior, away from the occiput, when you pull the occiput superior.
For working with the dural tube of the neck, have the person supine. Place the pads of the fingers of a monitoring hand on the tips of the cervical spinous processes and have the other hand under the occiput. Have the client’s head in neutral with respect to cervical flexion and extension, neither chin down nor chin up. This will put the plane of the face near parallel with the table. Draw the occiput straight superior with the occipital hand while monitoring cervical spinous processes with your other hand. Do not let the chin go posterior or anterior, which would represent flexion or extension of the neck.
Just like other areas of the spine, if there is no dural tube adhesion, the cervical spinous processes will spread open superiorly in an even way. If there is a posterior dural tube adhesion, the spinous process of that vertebra will move superior faster than its neighbors. If the dural tube adhesion is anterior in the neural canal, the spinous process will move inferior with respect to its neighbors. As with pulls from the sacrum, this can only be assessed while you are moving the occiput superior. Once the occiput is in a more superior position, there is nothing to feel.
Treatment in the neck is the same as what was described for the lumbar area, with the understanding that if the problem is perceived at the level of C1, C2, or C3, then, because the dural tube naturally adheres to these vertebrae, you are treating a contracture in the dural tube between adjacent vertebrae rather than an adhesion to the periosteum within a vertebra.
Jeffrey Burch received bachelor’s degrees in biology and psychology, and a master’s degree in counseling from the University of Oregon. He was certified as a Rolfer in 1977 and completed his advanced Rolfing® Structural Integration certification in 1990. Burch studied cranial manipulation in three different schools, including with French osteopath Alain Gehin. Starting in 1998, he began studying visceral manipulation with Jean-Pierre Barral, DO, and his associates, completing the apprenticeship to teach visceral manipulation. Although no longer associated with the Barral Institute, Burch has Barral’s permission to teach visceral manipulation. Having learned assessment and treatment methods in several osteopathically derived schools, he developed several new assessment and treatment methods that he now teaches, along with established methods. In recent years, he has developed original methods for assessing and releasing fibrosities in joint capsules, bursas, and tendon sheaths. He is also beginning to teach these new methods. Burch, as the founding editor of the IASI Yearbook, regularly contributes to it, as well as to other journals.
References
Kekere, Victor, and Khalid Alsayouri. 2023. Anatomy, head and neck, dura mater. In: StatPearls [Internet]. Treasure Island, Florida: StatPearls Publishing. Available from https://www.ncbi.nlm.nih.gov/books/NBK545301/.
Ünal, Mehmet, and Ahmet Burak Sezgin. 2021. Dura mater: Anatomy and clinical implications. Journal of Behavioral and Brain Science 11(10):239-247.
Keywords
dural tube adhesions; structural integration; manual therapy; fascial adhesions; spinal mobility; whiplash injuries; meningitis; neural canal biomechanics; sacral traction; occipital traction; vertebrae; craniosacral manipulation ■
View all articles: Articles home



